Physicians disproportionately suffer from substance use disorder. Is this phenomenon causal?
Based on research by D. Mark Anderson, Ron Diris, Raymond Montizaan, and Daniel I. Rees.
Physicians tend to enjoy good physical health. The typical physician exercises more, is less likely to smoke and is less likely to be obese than his or her non-physician counterpart (Nelson et al. 1994; Frank et al. 1998; Abramson et al. 2000; John and Hanke 2003; Smith and Leggat 2007; Leuven et al. 2013). In the United States, physicians live an average of two years longer than other professionals and almost three years longer than members of the general population (Frank et al. 2000).
Although physically healthy, there is evidence that physicians disproportionately suffer from mental health problems and substance use disorder (SUD). More than 20 percent of physicians are depressed or exhibit the symptoms of depression (Mata et al. 2015; Rotenstein et al. 2018, eTable 24); 10 to 15 percent of physicians will misuse alcohol or prescription drugs during their career (Baldisseri 2007; Vayr et al. 2019); and at least one-third of physicians describe themselves as suffering from “job burnout” (Drummond 2015), a syndrome that is closely linked to depression and SUDs (Bianchi et al. 2015; Schonfeld and Bianchi 2016; Wurm et al. 2016; Stageberg et al. 2020). Compounding these problems, physicians are often reluctant to seek psychological help, perhaps out of shame or fear of losing their license (Dyrbye et al. 2017; Tay et al. 2018; Weiner 2020; Belluz 2021).
Could becoming a physician lead, in a causal sense, to mental health problems and SUDs? Answering this question is important from a policy perspective. If, for instance, easy access to prescription drugs and the rigors of residency encourage physicians to abuse substances, then concrete steps can be taken to shield them. If, on the other hand, physicians are somehow predisposed to SUDs—if, for instance, their drug abuse is entirely explained by personality or other individual-level traits—then protecting them against malpractice claims will do nothing to solve the problem.
In a recently released working paper (Anderson et al. 2021), we explore the effect of becoming a physician on antidepressant use and other prescription drugs such as anxiolytics, sedatives, and opioids. Anxiolytics and sedatives include a range of benzodiazepines (e.g., Xanax and Versed) that are popular among physicians seeking self-treatment (Moberly 2014; Khan et al. 2019). Similar to Oxycodone and other prescription opioids, benzodiazepines are addictive and come with an extremely high potential for abuse (American Addiction Centers 2021).
Our data are from the Netherlands, where the number of students admitted to medical school is tightly regulated: applicants outnumber available slots, and acceptance to medical school is determined at random, based on the results of an annual admissions lottery. Following Leuven et al. (2013) and Ketel et al. (2016) and Artmann et al. (2021), we use the outcomes from these annual admissions lotteries as an instrumental variable (IV), allowing us to credibly distinguish the effect of becoming a physician from the effects of difficult-to-observe individual-level traits such as intelligence, personality and perseverance, all of which are potentially correlated with the decision to become a physician, mental health, and substance use (Ashby et al. 2006; White et al. 2012; Lo and Abbott 2013; Karpinski et al. 2018; Leung et al. 2019; Eley et al. 2020).
Data on lottery outcomes for 27,464 of medical school applicants were obtained from the Dienst Uitvoering Onderwijs, a Dutch governmental organization under the Ministry of Education. We observe the outcomes of all medical school lotteries conducted between 1987 and 1999. (After 1999, the national lottery was replaced with a decentralized selection system that gave medical schools more control over the admissions process.) Data on each applicant’s prescription drug use for the period 2006-2018 came from the Dutch prescription reimbursement database provided by Statistics Netherlands.
Becoming a physician and antidepressant use
Our IV estimates indicate that applicants induced into becoming physicians by winning the admissions lottery are more likely to use prescription antidepressants than those who lose the lottery and go into a different profession. Specifically, we find that becoming a physician leads to a 0.029 increase in the probability of having been prescribed an antidepressant during the period 2006-2018, which represents 23 percent increase relative to the sample mean (Figure 1).
Figure 1: Prescription Drug Use among Physicians vs. Non-Physicians: Pooled Sample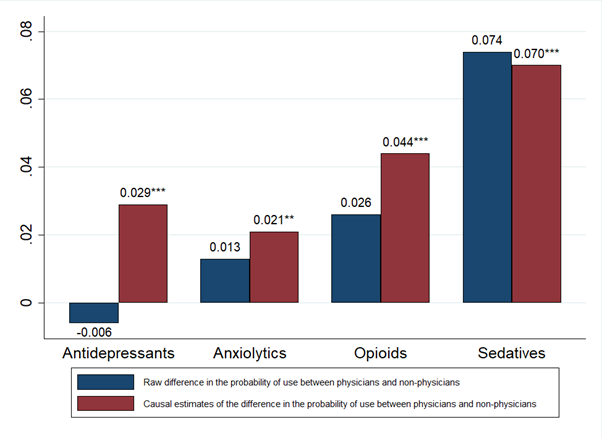 Notes: The sample is composed of 27,464 first-time medical school applicants in the Netherlands. Prescription drug use is for the period 2006-2018. Causal (i.e., IV) estimates are based on a regression model in which becoming a physician is instrumented using medical school lottery outcomes. IV estimates of the effect of becoming a physician control for gender, age at first lottery, lottery category fixed effects, year-of-first-lottery fixed effects, and lottery category by year-of-first-lottery fixed effects. *Statistically significant at 10% level; ** at 5% level; *** at 1% level.
Notes: The sample is composed of 27,464 first-time medical school applicants in the Netherlands. Prescription drug use is for the period 2006-2018. Causal (i.e., IV) estimates are based on a regression model in which becoming a physician is instrumented using medical school lottery outcomes. IV estimates of the effect of becoming a physician control for gender, age at first lottery, lottery category fixed effects, year-of-first-lottery fixed effects, and lottery category by year-of-first-lottery fixed effects. *Statistically significant at 10% level; ** at 5% level; *** at 1% level.
The medical literature describes female physicians as being at elevated risk for substance use disorder and depression (Oreskovich et al. 2015; Guille et al. 2017) and estimates from meta-analyses show that female physicians commit suicide at much higher rates than male physicians (Schernhammer and Colditz 2004; Duarte et al. 2020). When we split our sample by gender, becoming a physician leads to a 0.042 increase in the probability of having been prescribed an antidepressant among female applicants (Figure 2). Although also positive, the corresponding IV estimate for male applicants is much smaller and is nowhere near statistically significant at conventional levels (Figure 3).
Figure 2: Prescription Drug Use among Physicians vs. Non-Physicians: Sample Restricted to Female Applicants 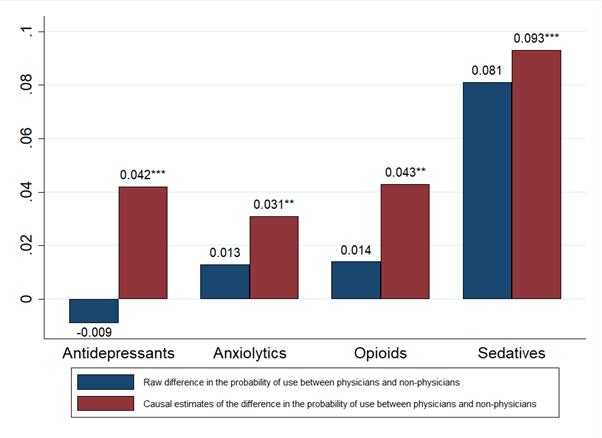 Notes: The sample is composed of 15,896 female first-time medical school applicants in the Netherlands. Prescription drug use is for the period 2006-2018. Causal (i.e., IV) estimates are based on a regression model in which becoming a physician is instrumented using medical school lottery outcomes. IV estimates of the effect of becoming a physician control for age at first lottery, lottery category fixed effects, year-of-first-lottery fixed effects, and lottery category by year-of-first-lottery fixed effects. *Statistically significant at 10% level; ** at 5% level; *** at 1% level.
Notes: The sample is composed of 15,896 female first-time medical school applicants in the Netherlands. Prescription drug use is for the period 2006-2018. Causal (i.e., IV) estimates are based on a regression model in which becoming a physician is instrumented using medical school lottery outcomes. IV estimates of the effect of becoming a physician control for age at first lottery, lottery category fixed effects, year-of-first-lottery fixed effects, and lottery category by year-of-first-lottery fixed effects. *Statistically significant at 10% level; ** at 5% level; *** at 1% level.
Figure 3: Prescription Drug Use among Physicians vs. Non-Physicians: Sample Restricted to Male Applicants 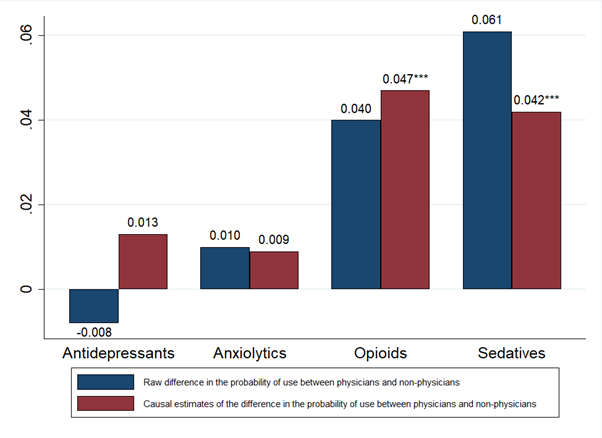 Notes: The sample is composed of 11,568 male first-time medical school applicants in the Netherlands. Prescription drug use is for the period 2006-2018. Causal (i.e., IV) estimates are based on a regression model in which becoming a physician is instrumented using medical school lottery outcomes. IV estimates of the effect of becoming a physician control for age at first lottery, lottery category fixed effects, year-of-first-lottery fixed effects, and lottery category by year-of-first-lottery fixed effects. *Statistically significant at 10% level; ** at 5% level; *** at 1% level.
Notes: The sample is composed of 11,568 male first-time medical school applicants in the Netherlands. Prescription drug use is for the period 2006-2018. Causal (i.e., IV) estimates are based on a regression model in which becoming a physician is instrumented using medical school lottery outcomes. IV estimates of the effect of becoming a physician control for age at first lottery, lottery category fixed effects, year-of-first-lottery fixed effects, and lottery category by year-of-first-lottery fixed effects. *Statistically significant at 10% level; ** at 5% level; *** at 1% level.
Becoming a physician and the use of anxiolytics, opioids, and sedatives
Why does becoming a physician increase antidepressant use among female medical school applicants? It is possible that something intrinsic to the profession causes poor mental health and antidepressant use. However, our IV estimates provide evidence that becoming a physician increases the use of types of other prescription drugs, not just antidepressants. In our pooled sample (i.e., the sample composed of both male and female applicants), becoming a physician leads to a 0.021 increase in the probability of having been prescribed an anxiolytic (Figure 1). This estimate is 20 percent of the sample mean and is, in fact, more than large enough to explain the unadjusted (i.e., the “raw”) gap in anxiolytic use between physicians and non-physicians. Becoming a physician is also associated with a 0.044 increase in the probability of having been prescribed an opioid (which is 25 percent of the sample mean), and a 0.070 increase in the probability of having been prescribed a sedative (which is 61 percent of the sample mean). Again, these IV estimates can explain the entire unadjusted gaps between physicians and non-physicians.
Among female applicants, becoming a physician leads to a 0.031 increase in the probability of having been prescribed an anxiolytic, or 27 percent of the mean (Figure 2). Female applicants who were induced into becoming a physician by winning the lottery were also more likely to use prescription opioids and much more likely to use prescription sedatives than their counterparts who lost the lottery and went into another profession. Restricting the sample to male applicants produces positive, but considerably smaller, IV estimates for anxiolytics and sedatives (Figure 3). Among male applicants, becoming a physician is associated with a 0.047 increase in the probability of having been prescribed an opioid (or 28 percent of the mean), which is comparable to the estimated effect among female applicants.
Summing up
We view the sizeable increases in the use of anxiolytics (e.g., Xanax), opioids (e.g., Oxycodone), and sedatives (e.g., Versed) among physicians in our sample as particularly worrisome. These drugs are highly addictive and there is descriptive evidence that they are often abused by physicians (Merlo and Gold 2008; Oaklander 2015; Moberly 2014; Khan et al. 2019). Although we cannot distinguish legitimate use from misuse in our data, it is clear that Dutch physicians are especially prone to using prescription drugs, a phenomenon that is entirely explained by their choice of profession as opposed to their personality or other difficult-to-observe individual-level traits.
Further Reading:
Anderson, D. Mark, Ron Diris Raymond Montizaan Daniel I. Rees. 2021. “The Effects of Becoming a Physician on Prescription Drug Use and Mental Health Treatment.” IZA DP No. 14890.
https://www.iza.org/publications/dp/14890/the-effects-of-becoming-a-physician-on-prescription-drug-use-and-mental-health-treatment
About the authors:
Mark Anderson is a Professor in the Department of Agricultural Economics and Economics, Montana State University.
https://www.montana.edu/econ/directory/1523860/dmark-anderson
Ron Diris is an Assistant Professor in the Department of Economics, Leiden University.
https://www.universiteitleiden.nl/en/staffmembers/ron-diris#tab-1
Raymond Montizaan is a senior researcher at the Research Centre for Education and the Labour Market (ROA), Maastricht University.
https://www.maastrichtuniversity.nl/r.montizaan
Daniel I. Rees is a Professor in the Department of Economics, Universidad Carlos III de Madrid.
http://economics.uc3m.es/personal/rees/
References:
Abramson, Scott, Joel Stein, Michael Schaufele, Elizabeth Frates, and Shannon Rogan. 2000.
“Personal Exercise Habits and Counseling Practices of Primary Care Physicians: A National Survey.” Clinical Journal of Sport Medicine, 10(1): 40-48.
American Addiction Centers. 2021. “Benzodiazepine Addiction: Symptoms & Signs of Dependence.” Available at: https://americanaddictioncenters.org/benzodiazepine/symptoms-and-signs.
Artmann, Elisabeth, Hessel Oosterbeek, and Bas van der Klaauw. 2021. “Do Doctors Improve the Health Care of Their Parents? Evidence from Admission Lotteries.” American Economic Journal: Applied Economics, In Press.
Ashby, Jeffrey S., Kenneth G. Rice, and James L. Martin. 2006. “Perfectionism, Shame, and Depressive Symptoms.” Journal of Counseling and Development, 84(2): 148-156.
Baldisseri, Marie. 2007. “Impaired Healthcare Profession.” Critical Care Medicine, 35(2 Suppl.): S106-S116.
Bianchi, Renzo, Irvin Sam Schonfeld, and Eric Laurent. 2015. “Burnout–Depression Overlap: A Review.” Clinical Psychology Review, 36: 28–41.
Belluz, Julia. 2021. “The Doctors are Not All Right.” Vox, Jun 23. Available at: https://www.vox.com/22439911/doctors-mental-health-suicide-coronavirus-pandemic
Caruso, Stephen. 2020. “Wolf Signs Executive Order Shielding Some Healthcare workers against Malpractice Claims during Pandemic.” Pennsylvania Capital Star, May 6. Available at: https://www.penncapital-star.com/blog/wolf-signs-executive-order-shielding-healthcare-workers-against-malpractice-claims-during-pandemic/.
Drummond, Dike. 2015. “Physician Burnout: Its Origin, Symptoms, and Five Main Causes.” Family Practice Management, 22(5): 42-47.
Duarte, Dante, Mirret M. El-Hagrassy, Tiago Castro e Couto, Wagner Gurgel, Felipe Fregni, and Humberto Correa. 2020. “Male and Female Physician Suicidality: A Systematic Review and Meta-analysis.” JAMA Psychiatry, 77(6): 587-597.
Dyrbye, Liselotte, Colin West, Christine Sinsky, Lindsey Goeders, Daniel Satele, and Tait Shanafelt. 2017. “Medical Licensure Questions and Physician Reluctance to Seek Care for Mental Health Conditions.” Mayo Clinic Proceedings, 92(10): 1486-1493.
Eley, Diann S., Vikas Bansal, and Janni Leung. 2020. “Perfectionism as a Mediator of Psychological Distress: Implications for Addressing Underlying Vulnerabilities to the Mental Health of Medical Students.” Medical Teacher, 42(11): 1301–1307.
Frank, Erica, Holly Biola, and Carol Burnett. 2000. “Mortality Rates and Causes Among U.S. Physicians.” American Journal of Preventative Medicine, 19(3): 155-159.
Frank, Erica, Donna Brogan, Ali Mokdad, Eduardo Simoes, Henry Kahn, and Raymond Greenberg. 1998. “Health-Related Behaviors of Women Physicians vs. Other Women in the United States.” Archives of Internal Medicine, 158(4): 342-348.
Guille, Constance, Elena Frank, Zhuo Zhao, David A. Kalmbach, Paul J. Nietert, Douglas A. Mata, and Srijan Sen. 2017. “Work-Family Conflict and the Sex Difference in Depression Among Training Physicians” JAMA Internal Medicine, 177(12): 1766-1772.
John, U., and M. Hanke. 2003. “Tobacco-Smoking Prevalence among Physicians and Nurses in Countries with Different Tobacco-Control Activities.” European Journal of Cancer Prevention, 12(3): 235–237.
Karpinski, Ruth, Audrey Kinase Kolba, Nicole Tetreault, and Thomas Borowski. 2018 “High Intelligence: A Risk Factor for Psychological and Physiological Overexcitabilities.” Intelligence, 66: 8-23.
Ketel, Nadine, Edwin Leuven, Hessel Oosterbeek, Bas van der Klaauw “The Returns to Medical School: Evidence from Admission Lotteries.” American Economic Journal: Applied Economics, 8 (2): 225-254.
Khan, Aftab Alam, Imtiaz Ud Din, Adil Naseer Khan, Imranullah Khan, Humaira Hanif, and Haq Nawaz. 2019. “Benzodiazepine Use among Resident Doctors in Tertiary Care Hospital.” Journal of Ayub Medical College, 31(4): 553-557.
Leuven, Edwin, Hessel Oosterbeek, and Inge de Wolf. 2013. “The Effects of Medical School on Health Outcomes: Evidence from Admission Lotteries.” Journal of Health Economics, 32(4): 698-707.
Lo, Alice and Maree J. Abbott. 2013. “Review of the Theoretical, Empirical, and Clinical Status of Adaptive and Maladaptive Perfectionism.” Behaviour Change, 30(2): 96-116
Leung, Janni, C. Robert Cloninger, Barry Hong, Kevin Cloninger, and Diann Eley. 2019. “Temperament and Character Profiles of Medical Students Associated with Tolerance of Ambiguity and Perfectionism.” PeerJ, 7: e7109.
Mata, Douglas A., Marco A. Ramos, Narinder Bansal, Rida Khan, Constance Guille, Emanuele Di Angelantonio, and Srijan Sen. 2015. “Prevalence of Depression and Depressive Symptoms Among Resident Physicians: A Systematic Review and Meta-analysis.” JAMA, 314(22): 2373–2383.
Merlo, Lisa and Mark Gold. 2008. “Prescription Opioid Abuse and Dependence among Physicians: Hypotheses and Treatment.” Harvard Revivew of Psychiatry, 16(3): 181-194.
Nelson, David, Gary Giovino, Seth Emont, Robert Brackbill, Lorraine Cameron, John Peddicord, and Paul Mowery. 1994. “Trends in Cigarette Smoking among US Physicians and Nurses.” JAMA, 271(16): 1273-1275.
Oaklander, Mandy. 2015. “Doctors on Life Support.” Time, August 27. Available at: https://time.com/4012840/doctors-on-life-support/.
Oreskovich Michael R., Tait Shanafelt, Lotte N. Dyrbye, Litjen Tan, Wayne Sotile, Daniel Satele BS, Colin P. West, Jeff Sloan, and Sonja Boone. 2015. “The Prevalence of Substance Use Disorders in American Physicians.” American Journal on Addictions, 24(1): 30-38.
Rotenstein, Lisa S., Matthew Torre, Marco A. Ramos, Rachael C. Rosales, Constance Guille, Srijan Sen, and Douglas A. Mata. 2018. “Prevalence of Burnout Among Physicians: A Systematic Review.” JAMA, 320(11): 1131-1150.
Schernhammer, Eva and Graham A. Coldtiz. 2004. “Suicide Rates among Physicians: A Quantitative and Gender Assessment (Meta-Analysis).” American Journal of Psychiatry, 161(12): 2295-302.
Schonfeld, Irvin and Renzo Bianchi. 2016. “Burnout and Depression: Two Entities or One?” Journal of Clinical Psychology, 72(1): 22-37.
Smith, Derek and Peter Leggat. 2007. “An International Review of Tobacco Smoking in the Medical Profession: 1974–2004.” BMC Public Health, 7: Article 115.
Stageberg, Elaine L, Amy L. Stark, and Katherine M. Moore. 2020. “Rates of Burnout, Depression, Suicide, and Substance Use Disorders.” In Cynthia Stonnington and Julia Files (eds.), Burnout in Women Physicians. Cham, Switzerland: Springer.
Tay, Stacie, Kat Alcock, and Katrina Scior. 2018. “Mental Health Problems Among Clinical Psychologists: Stigma and its Impact on Disclosure and Help-Seeking.” Journal of Clinical Psychology, 74(9): 1545-1555.
Vayr, Flora, Fabrice Herin, Benedicte Jullian, Jean Marc Soulat, and Nicolas Franchitto. “Barriers to Seeking Help for Physicians with Substance Use Disorder: A Review.” Drug and Alcohol Dependence, 199: 116-121.
Weiner, Stacy. 2020. “Doctors Forgo Mental Health Care During Pandemic Over Concerns about Licensing, Stigma.” Association of American Medical Colleges, December 10. Available at: https://www.aamc.org/news-insights/doctors-forgo-mental-health-care-during-pandemic-over-concerns-about-licensing-stigma.
White, James, Catharine Gale, and G. David Batty. 2012. “Intelligence Quotient in Childhood and the Risk of Illegal Drug Use in Middle-Age: The 1958 National Child Development Survey.” Annals of Epidemiology, 22(9): 654-657.
Wurm, Walter, Katrin Vogel, Anna Holl, Christoph Ebner, Dietmar Bayer, Sabrina Mörkl, Istvan-Szilard Szilagyi, Erich Hotter, Hans-Peter Kapfhammer, and Peter Hofmann. 2016. “Depression-Burnout Overlap in Physicians.” PLoS ONE, 11(3): e0149913.